- More Than Distant Organs
- A Conversation Beneath the Surface
- What Shows Up on the Skin, Starts in the Gut
- Microbial Messengers in Motion
- The BB536 and M-16V Effect: Nurturing Balance from Within
- Dysbiosis and the Skin Fallout
- When the Gut Speaks in Phenols: Another Link to Skin Health
- Final Word: Your Skin Reflects Your Gut Microbiome Well-Being
How your microbiome shapes what shows up in the mirror,
and how Skinbiotica helps nurture radiance from within.
More Than Distant Organs
Your skin and gut are more than distant organs. They share astonishing resemblances: both are lined by epithelial cells that act as protective barriers. They are also richly vascularised and innervated, allowing rapid communication with immune and central nervous system, in order to facilitate rapid responses to environmental threat. The gut-skin axis results from this resemblance [1]. It refers to the dynamic relationship between the gut microbiota, the immune system, and the skin.
A Conversation Beneath the Surface
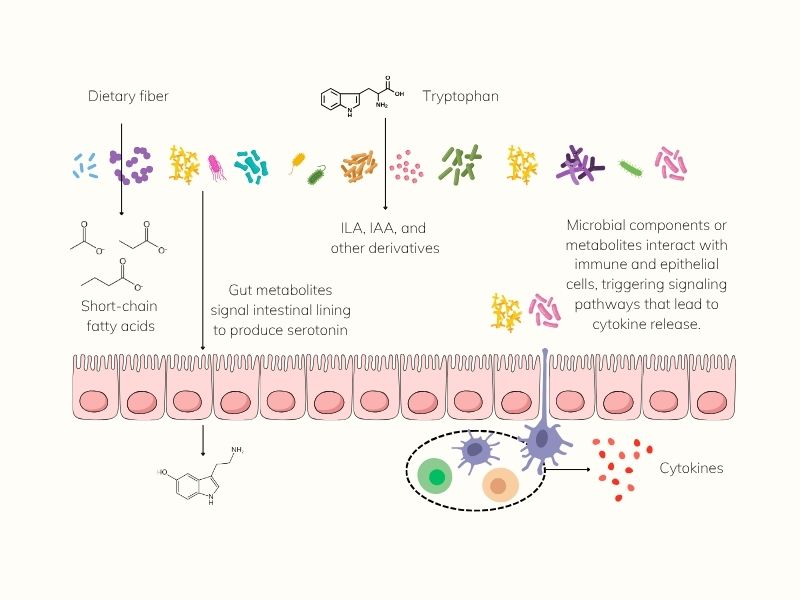
Skin health isn’t just skin deep. While the gut and skin may seem like separate systems, they’re in constant biochemical conversation, communicating through cytokines [2], hormones [3], and microbial metabolites like short-chain fatty acids (SCFAs) [4] and tryptophan derivatives.
This internal dialogue helps regulate everything from inflammation and immune response to hydration and barrier repair. When the gut is balanced, these signals support clarity, calm, and resilience on the skin’s surface. When the gut is disrupted, the skin often speaks up with breakouts, dryness, premature aging, or chronic inflammation [5].
From gut to glow: How microbial messengers shape skin health from within.
What Shows Up on the Skin, Starts in the Gut
Emerging research continues to show how specific patterns in gut microbiota correlate with common skin conditions. In acne, eczema, and psoriasis, scientists have observed shifts in microbial composition: reduced diversity, depletion of beneficial species, or increases in potentially harmful strains. These may drive inflammation, compromise barrier function, or disrupt immune regulation.
We highlight these associations below, offering a snapshot of the gut-skin axis in three of the most prevalent inflammatory skin disorders.
From acne to eczema to psoriasis, disruptions in the gut microbiome often mirror the skin’s distress. Research highlights specific microbial changes, like reduced Bifidobacterium in acne and eczema, or decreased Akkermansia in psoriasis, that point to impaired barrier function, inflammation, and diminished resilience. Restoring microbial balance may offer a path toward skin health, from the inside out.

Microbial Messengers in Motion
One of the most important players in this exchange is butyrate, a gut-derived SCFA. It helps reduce systemic inflammation, strengthens epithelial integrity, and supports immune regulation, key in managing inflammatory skin conditions like acne, eczema, and rosacea [5].
Other gut metabolites affect the skin more directly. Propionic acid, for instance, has been shown to suppress the growth of Staphylococcus aureus, a common skin pathogen implicated in eczema and other flare-ups [12].
The story continues with tryptophan metabolites, compounds produced by gut microbes when they process the amino acid tryptophan. Among these, indole-3-lactic acid (ILA) and indole-3-acetic acid (IAA) stand out [13]. They activate the aryl hydrocarbon receptor (AhR), a key regulator of skin immunity and barrier repair [14]. Dysregulation of this receptor has been implicated in psoriasis and atopic dermatitis [15,16], while reduced AhR activity is also observed in the gut microbiota of individuals with inflammatory bowel disease [17].
Importantly, ILA-mediated activation of AhR has been shown to reduce inflammation and enhance barrier integrity in both the gut and skin epithelia, underscoring the deeply intertwined nature of these two organs [18,19].
And it’s not just any microbes that do this work. Infant-type Bifidobacteria, including B. longum, B. breve, and B. bifidum, are among the most effective ILA producers [20,21].

The BB536 and M-16V Effect: Nurturing Balance from Within
At AB INTRA, we craft our formulations to support the gut-skin axis where it begins: within the microbiome.
Take Bifidobacterium longum BB536, an infant-type, human-residential strain known for its ability to foster microbial harmony and produce beneficial metabolites. In a double-blind, placebo-controlled trial [20], participants who consumed fermented milk enriched with BB536 showed:
- A significant increase in beneficial microbes like Faecalibacterium
- Elevated levels of tryptophan, and its key derivatives: indole-3-lactic acid (ILA), indole-3-acetic acid (IAA), and indole-3-aldehyde (IAld), which help strengthen skin and gut barriers via AhR activation
- A clear correlation between BB536 colonization and the production of these skin-relevant metabolites
These findings suggest that BB536 does more than balance the gut. It actively contributes to the molecular crosstalk that influences immune response, barrier integrity, and visible skin calm.
To complement its effects, we include Bifidobacterium breve M-16V, another clinically studied, human-residential strain. Together, these two probiotics, which are featured in Skinbiotica COLLAGEN+, have been shown to help modulate the gut-skin axis and support skin firmness [23,24].
It’s a synergistic pairing that works from the inside out, nourishing your microbiome and helping your skin reflect its inner balance.g
Dysbiosis and the Skin Fallout
When gut microbial balance is disturbed, known as dysbiosis, it may trigger a cascade that can impair skin health:
- Leaky gut increases the passage of unwanted molecules into the bloodstream, activating immune responses that show up on the skin.
- Low microbial diversity can reduce SCFA production, compromising both gut and skin barrier function.
- Chronic inflammation, driven by poor gut health, can disrupt collagen synthesis and accelerate visible signs of aging.
The solution isn’t found in one miracle molecule, it begins with restoring balance at the core. This is why the concept of “beauty from within” is no longer just a philosophy, it’s backed by science. And it’s why supporting your gut with targeted strains like BB536 and M-16V may do more for your skin than the most expensive cream ever could.

Interlude: Kitava, the Acne-Free Island
On the remote island of Kitava in Papua New Guinea, a remarkable study unfolded. Over three years, researcher Staffan Lindeberg closely observed 1,200 islanders, including 300 adolescents aged 15 to 25. What made this group extraordinary? At the time, their diet remained untouched by Western influence, reflecting the ancestral patterns our microbiome co-evolved with. Their daily meals consisted mainly of tropical fruits, root vegetables, coconut, and fresh fish: foods rich in fermentable fiber and omega-3s, yet naturally low in refined sugars, processed foods, and additives.
The results were astonishing. Not only were heart disease and stroke virtually nonexistent, but so was acne. Not a single case [22].
This striking absence of acne raised a compelling question: could modern skin concerns be, at least in part, a byproduct of what we leave out or include in our diets? In Kitava, where fiber intake was high and gut microbiomes likely diverse and well-nourished, skin health was simply… untroubled.
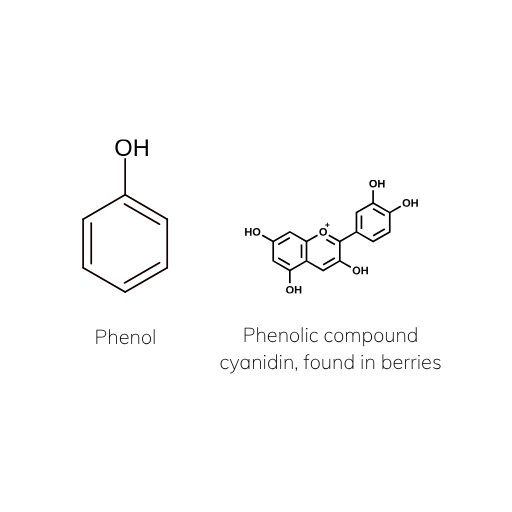
Not All “Phenols” Are the Same
It’s easy to confuse phenol and phenolic compounds, but their effects on your body couldn’t be more different.
Phenol and p-cresol are byproducts of protein fermentation, associated with disrupted skin barrier function, dryness, and inflammation. Elevated levels are often signs of gut imbalance.
By contrast, phenolic compounds are plant-derived metabolites found in colorful fruits, vegetables, teas, and spices. These polyphenols can support gut health by promoting beneficial microbes and reducing oxidative stress and inflammation.
When the Gut Speaks in Phenols: Another Link to Skin Health
Not all microbial metabolites are beneficial. Phenols, including phenol and p-cresol, are byproducts of aromatic amino acid fermentation by gut bacteria. These compounds that have been directly associated with disrupted skin barrier function and dryness [23].
Research has identified several phenol-producing species, such as Proteus, Streptococcus faecalis, Bacteroides fragilis, Fusobacterium, and Clostridium spp., particularly under unfavorable gut conditions, like increased alkalinity [24]. Because of this, phenols are often used as biomarkers for gut environment quality [25].
But the skin doesn’t escape their effects. Phenols produced in the gut can enter systemic circulation and accumulate in the skin, where they’ve been shown to disrupt keratinocyte differentiation in animal models [26]. In other words, what happens in the gut can compromise the skin’s ability to renew and protect itself.
There’s good news: prebiotics like galacto-oligosaccharides (GOS) can help shift the balance.
Studies show that GOS reduces phenol production by promoting beneficial microbial activity. In human trials, GOS intake prevented water and keratin loss in women whose skin had been affected by phenolic metabolites [27]. In animal studies, GOS even blocked the development of atopic dermatitis, likely through its ability to induce the anti-inflammatory cytokine IL-10 and inhibit IL-17 [28].
The benefits grow stronger in synergy. The combination of GOS and Bifidobacteria, like those in Skinbiotica COLLAGEN+, has been clinically shown to improve skin conditions by reducing inflammatory markers and phenol-related skin disruptions [26,27,29].
Quiet the chaos. Nourish what calms. By reducing the production of harmful metabolites like phenols, you’re not just feeding your microbiome. You’re supporting skin from the inside, where balance begins.
Final Word: Your Skin Reflects Your Gut Microbiome Well-Being
Great skin isn’t built overnight. And it certainly isn’t built on serums alone. It’s the result of a well-fed, well-balanced microbiome that sends out calming, nourishing signals from the inside out.
At AB INTRA, we honour this intricate gut-skin dialogue with targeted formulations that support microbial harmony and metabolite production, right where it matters most.
Skinbiotica COLLAGEN+ was crafted with this science in mind. With clinically studied probiotics like B. longum BB536 and B. breve M-16V, and prebiotic GOS to nourish them, this formula helps your gut do what it was designed to: support immune balance, reduce inflammation, and promote radiant skin naturally.
Because when the gut is nourished, the skin follows.
References
C. A. O’Neill, G. Monteleone, J. T. McLaughlin, and R. Paus, “The gut-skin axis in health and disease: A paradigm with therapeutic implications,” BioEssays, vol. 38, no. 11, pp. 1167–1176, Nov. 2016, doi: https://doi.org/10.1002/bies.201600008.
T. Nakatsuji et al., “Staphylococcus aureus Exploits Epidermal Barrier Defects in Atopic Dermatitis to Trigger Cytokine Expression,” J. Invest. Dermatol., vol. 136, no. 11, pp. 2192–2200, Nov. 2016, doi: 10.1016/j.jid.2016.05.127.
A. Sadiq et al., “The Role of Serotonin during Skin Healing in Post-Thermal Injury,” International Journal of Molecular Sciences, vol. 19, no. 4. 2018, doi: 10.3390/ijms19041034.
X. Xiao et al., “The role of short-chain fatty acids in inflammatory skin diseases,” Front. Microbiol., vol. Volume 13, 2023. DOI: 10.3389/fmicb.2022.1083432
B. De Pessemier, L. Grine, M. Debaere, A. Maes, B. Paetzold, and C. Callewaert, “Gut–Skin Axis: Current Knowledge of the Interrelationship between Microbial Dysbiosis and Skin Conditions,” Microorganisms, vol. 9, no. 2. 2021, doi: 10.3390/microorganisms9020353.
H.-M. Yan, H.-J. Zhao, D.-Y. Guo, P.-Q. Zhu, C.-L. Zhang, and W. Jiang, “Gut microbiota alterations in moderate to severe acne vulgaris patients,” J. Dermatol., vol. 45, no. 10, pp. 1166–1171, Oct. 2018, doi: https://doi.org/10.1111/1346-8138.14586.
Y. Deng, H. Wang, J. Zhou, Y. Mou, G. Wang, and X. Xiong, “Patients with Acne Vulgaris Have a Distinct Gut Microbiota in Comparison with Healthy Controls,” Acta Derm. Venereol., vol. 98, no. 8 SE-Articles, pp. 783–790, May 2018, doi: 10.2340/00015555-2968.
S. Watanabe et al., “Differences in fecal microflora between patients with atopic dermatitis and healthy control subjects,” J. Allergy Clin. Immunol., vol. 111, no. 3, pp. 587–591, Mar. 2003, doi: 10.1067/mai.2003.105.
H. Song, Y. Yoo, J. Hwang, Y.-C. Na, and H. S. Kim, “Faecalibacterium prausnitzii subspecies–level dysbiosis in the human gut microbiome underlying atopic dermatitis,” J. Allergy Clin. Immunol., vol. 137, no. 3, pp. 852–860, 2016, doi: https://doi.org/10.1016/j.jaci.2015.08.021.
M. C. Buhaș et al., “Gut Microbiota in Psoriasis,” Nutrients, vol. 14, no. 14. 2022, doi: 10.3390/nu14142970.
L. Chen et al., “Skin and Gut Microbiome in Psoriasis: Gaining Insight Into the Pathophysiology of It and Finding Novel Therapeutic Strategies,” Front. Microbiol., vol. Volume 11-2020, 2020. https://doi.org/10.3389/fmicb.2020.589726
K. Chilicka, I. Dzieńdziora-Urbińska, R. Szyguła, B. Asanova, and D. Nowicka, “Microbiome and Probiotics in Acne Vulgaris—A Narrative Review,” Life, vol. 12, no. 3. 2022, doi: 10.3390/life12030422.
T. D. Hubbard et al., “Adaptation of the human aryl hydrocarbon receptor to sense microbiota-derived indoles,” Sci. Rep., vol. 5, no. 1, p. 12689, 2015, doi: 10.1038/srep12689.
N. Fernández-Gallego, F. Sánchez-Madrid, and D. Cibrian, “Role of AHR Ligands in Skin Homeostasis and Cutaneous Inflammation,” Cells, vol. 10, no. 11. 2021, doi: 10.3390/cells10113176.
J. E. Kim et al., “Aryl Hydrocarbon Receptor and Autophagy-Related Protein Microtubule-Associated Protein Light Chain 3 Expression in Psoriasis,” Ann Dermatol, vol. 33, no. 2, pp. 138–146, Apr. 2021. https://doi.org/10.5021/ad.2021.33.2.138
K. Kim, H. Kim, and G. Y. Sung, “Effects of Indole-3-Lactic Acid, a Metabolite of Tryptophan, on IL-4 and IL-13-Induced Human Skin-Equivalent Atopic Dermatitis Models,” International Journal of Molecular Sciences, vol. 23, no. 21. 2022, doi: 10.3390/ijms232113520.
B. Lamas et al., “CARD9 impacts colitis by altering gut microbiota metabolism of tryptophan into aryl hydrocarbon receptor ligands,” Nat. Med., vol. 22, no. 6, pp. 598–605, 2016, doi: 10.1038/nm.4102.
K. Yu et al., “Bacterial indole-3-lactic acid affects epithelium–macrophage crosstalk to regulate intestinal homeostasis,” Proc. Natl. Acad. Sci., vol. 120, no. 45, p. e2309032120, Nov. 2023, doi: 10.1073/pnas.2309032120.
P. Di Meglio et al., “Activation of the Aryl Hydrocarbon Receptor Dampens the Severity of Inflammatory Skin Conditions,” Immunity, vol. 40, no. 6, pp. 989–1001, Jun. 2014, doi: 10.1016/j.immuni.2014.04.019.
T. Sakurai, T. Odamaki, and J. Xiao, “Production of Indole-3-Lactic Acid by Bifidobacterium Strains Isolated fromHuman Infants,” Microorganisms, vol. 7, no. 9. 2019, doi: 10.3390/microorganisms7090340.
A. M. Ehrlich et al., “Bifidobacterium grown on human milk oligosaccharides produce tryptophan metabolite Indole-3-lactic acid that significantly decreases inflammation in intestinal cells in vitro,” FASEB J., vol. 32, no. S1, pp. lb359–lb359, Apr. 2018, doi: https://doi.org/10.1096/fasebj.2018.32.1_supplement.lb359.
L. Cordain, S. Lindeberg, M. Hurtado, K. Hill, S. B. Eaton, and J. Brand-Miller, “Acne Vulgaris: A Disease of Western Civilization,” Arch. Dermatol., vol. 138, no. 12, pp. 1584–1590, Dec. 2002, doi: 10.1001/archderm.138.12.1584.
R. Iizuka, K. Koji, I. Naoki, and K. and Chiba, “Phenols produced by gut bacteria affect the skin in hairless mice,” Microb. Ecol. Health Dis., vol. 21, no. 1, pp. 50–56, Jan. 2009, doi: 10.1080/08910600802688910.
E. A. Smith and G. T. Macfarlane, “Enumeration of human colonic bacteria producing phenolic and indolic compounds: effects of pH, carbohydrate availability and retention time on dissimilatory aromatic amino acid metabolism,” J. Appl. Bacteriol., vol. 81, no. 3, pp. 288–302, Sep. 1996, doi: https://doi.org/10.1111/j.1365-2672.1996.tb04331.x.
V. De Preter et al., “The in vivo use of the stable isotope-labelled biomarkers lactose-[15N]ureide and [2H4]tyrosine to assess the effects of pro- and prebiotics on the intestinal flora of healthy human volunteers,” Br. J. Nutr., vol. 92, no. 3, pp. 439–446, 2004, doi: DOI: 10.1079/BJN20041228.
K. Miyazaki, N. Masuoka, M. Kano, and R. Iizuka, “Bifidobacterium fermented milk and galacto-oligosaccharides lead to improved skin health by decreasing phenols production by gut microbiota,” Benef. Microbes, vol. 5, no. 2, pp. 121–128, 2014, doi: https://doi.org/10.3920/BM2012.0066.
M. KANO et al., “Consecutive Intake of Fermented Milk Containing Bifidobacterium breve Strain Yakult and Galacto-oligosaccharides Benefits Skin Condition in Healthy Adult Women,” Biosci. Microbiota, Food Heal., vol. 32, no. 1, pp. 33–39, 2013, doi: 10.12938/bmfh.32.33.
S. Tanabe and S. Hochi, “Oral administration of a galactooligosaccharide preparation inhibits development of atopic dermatitis-like skin lesions in NC/Nga mice,” Int J Mol Med, vol. 25, no. 3, pp. 331–336, 2010, doi: 10.3892/ijmm_00000349.
K.-B. Hong, J. Mingeum, H. Ki Soo, H. K. Jae, P. Yooheon, and H. J. and Suh, “Photoprotective effects of galacto-oligosaccharide and/or Bifidobacterium longum supplementation against skin damage induced by ultraviolet irradiation in hairless mice,” Int. J. Food Sci. Nutr., vol. 66, no. 8, pp. 923–930, Nov. 2015, doi: 10.3109/09637486.2015.1088823.
Next in Your Gut Health Journey
Explore further the fascinating world of gut health. Because better health is built one insight at a time.
Where Your Gut Meets Science
€ 269,85 Original price was: € 269,85.€ 214,95Current price is: € 214,95. incl. VAT
Consistency meets radiance. A 3-month supply of Skinbiotica COLLAGEN+—science-backed skin nutrition to support skin collagen, elasticity, and glow from within.
€ 209,90 Original price was: € 209,90.€ 179,95Current price is: € 179,95. incl. VAT
Complete beauty from within—Gutbiotica PRIME provides comprehensive microbiome support while Skinbiotica COLLAGEN+ promotes radiant and elastic skin.
€ 164,90 Original price was: € 164,90.€ 139,95Current price is: € 139,95. incl. VAT
A smart pairing for gut microbiome and weight support with Gutbiotica CORE and Fibersentials SHAPE to maintain a happy gut and support satiety naturally.







